Chapter 7: Sensory Examination
Author's Commentary
The sensory examination may be the most difficult and least objective part of the neurologic examination because most of it depends on the patients' response to a stimulus. Root, nerve, and false radiations due to visceral somatic convergence provide the sensory afference of the body surface. Roots and peripheral nerves are compressed or lesioned at specific anatomic points.
The molecular biology of pain and how it alters primary modalities of sensation, particularly mechanical and thermal afferences, are rapidly being unraveled. Alterations of neuropathic and inflammatory pain are reflected in clinical hyperalgesia, allodynia, and hyperpathia. These alterations occur from CNS lesions as well as peripheral tissue and nerve damage. Primary sensory modalities and discriminative touch are accomplished by sensory-motor circuitry. The limbic system provides the motivational and affectual components of sensation.
Excerpts From Chapter 7
This is the most difficult and least objective part of the neurologic examination because a major portion of it is under the control of the patient. However, the good examiner is armed with an understanding of the innervation patterns of the body surface, which are root, nerve or false radiations (somatic visceral convergence) or are central patterns of deficits that are reflected on the body surface. The nerve bundles themselves have a nervi-nervorum, which, if sensitized, causes pain when the bundle is compressed. Frequently, in radiculopathy, the muscle that receives innervation is sore from mechanical compression (sensitization) because nociceptive afferents which usually do not respond to simple pressure do so when they are sensitized. Thus, a disk that compresses the S1 root, which carries deep muscle pain afferents (A-delta fibers) causes the gastrocnemius muscle to hurt when compressed. This occurs because these A-delta receptors, which normally only respond to tissue-destructive stimuli, are now sensitized and respond to mechanical stimuli. Similarly, the same disk at S1 may sensitize the roots (L4–S2) in the sciatic notch so that when it is compressed, the patient feels pain at the notch, but not in other areas of the sciatic nerve innervation. Use of the thumb by the examiner on sensitized muscles and nerves, confirmed with careful observations of the patient, objectifies much of the sensory examination. Knowledge of the entrance points of the nerves through the thoracic inlet and outlet, the neurovascular bundle (medial to the humerus), and then the tunnels into the forearm (cubital, arcade of Frohse and the pronator canal) allows the examiner to palpate and judge the sensitivity of the nerves. Placing the plexus in specific positions (Roos' abduction stretch maneuver, Wright's maneuver) places different components of the plexus under traction and spontaneously fire. Compression of the cervical roots as they exit the cervical foramina (Spurling's maneuver) allows identification of specific nerve root irritation.
Examination Technique Demonstration
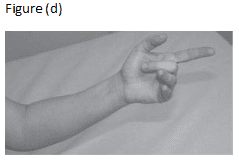
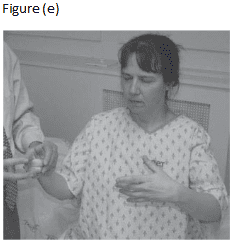
Fig. 7.2 Parietal copy. … (d) The position to be copied (reverse, as shown). (e) The patient appears confused and cannot copy the finger posture of the right hand (see text for details).
